By Sharada Saraf | SQ Online Reporter | SQ Online (2016-2017)
________________________________________________________________________________________
Every UCSD student knows the terror of waking up with a scratchy throat, knowing exactly what it implies: seven to ten days of actual torture, and the very real possibility of taking a midterm with a cold. The thought of dealing with being that kid who slumps across campus carrying a box of tissues, sniffles constantly during lecture, and coughs between every other sentence sends desperate students running to the market to find an end to their misery. The drug aisle, it seems, offers hope to any bleary-eyed college student searching for a quick fix to their dismal state.
Not so fast, say researchers at the University of Florida. In an editorial published in The Journal of Allergy and Clinical Immunology: In Practice, the UF scientists claimed that phenylephrine, a decongestant present in many popular over-the-counter medicines from Tylenol Sinus to Advil Sinus Congestion & Pain worked no better than a placebo at reducing nasal congestion when taken orally.
The editorial cited a study conducted by San Diego’s Allergy & Asthma Medical Group & Research Center, in which 539 adults were given phenylephrine from the Food and Drug Administration’s (FDA) approved level of 10 mg to a higher dose of 40 mg. The
researchers found that not only was 10 mg phenylephrine just as ineffective as a sugar pill at relieving congestion in the subjects, but it was also ineffective at levels four times the FDA-approved amount.
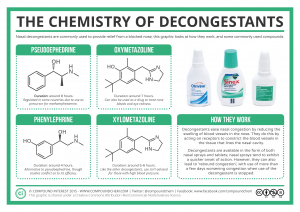
The doubt over the effectiveness of phenylephrine is nothing new: one study conducted by researchers from Germany’s University of Bonn found that the majority of the drug, broken down in the gut and liver, is flushed out of a person’s system before it can enter the bloodstream. Another 2009 study suggested that phenylephrine worked no better than a placebo: it appeared that pseudoephedrine, a medication that can only be obtained through a pharmacist, was the superior method in treating allergy-related congestion. The mechanism of action of the two compounds is slightly different, possibly making pseudoephedrine more effective in relaxing muscles in the airways to ease congestion: while pseudoephedrine targets multiple types of muscle receptors in the nasal cavity to reduce swelling, phenylephrine only acts on a single type of receptor.
So, if phenylephrine has been proven not to work at FDA-approved levels and beyond, why do we still use it?
The answer isn’t terribly surprising: drug companies don’t want a cut in their profits. If they choose to replace phenylephrine with the far more effective pseudoephedrine, they’d face serious losses by putting their products behind the counter. Drugs available on store shelves that claim to be effective in reducing congestants make up over $7.4 billion in annual profits, so companies are reluctant to break the image of phenylephrine as a safe and effective over-the-counter product.
While pseudoephedrine has more evidence supporting it as the more effective drug, increasing numbers of doctors have started to recommend that patients not take decongestants at all. This may be frustrating to those dealing with a stuffy nose, but decongestants often provide only short-term relief, and pose unpleasant side-effects like increased blood pressure, drowsiness, and dry mouth.
“The decongestants, in particular, I suspect most of us would not be the least bit surprised they’re not the least bit effective, because that’s our experience,” says Wanda Filer, president of the American Academy of Family Physicians. “Frequently, I find an awful lot of people may get an hour of relief; over the long term they seem to feel worse.”
So, for those of you who find yourselves in the midst of the sniffles, it appears that the best advice is…to let your colds run their course. Resist temptation, and don’t sink your money in over-the-counter decongestants. It’s exasperating that we still don’t have an effective medication to shorten the duration of the common cold or provide long-term alleviation of symptoms, but try to find comfort in the fact that your money may be better spent on a can of soup instead.
[hr gap=”30″]
Sources:
http://www.mayoclinic.org/drugs-supplements/phenylephrine-nasal-route/description/drg-20067912
http://www.mayoclinic.org/drugs-supplements/pseudoephedrine-oral-route/description/drg-20067942
https://www.drugbank.ca/drugs/DB00388
https://www.drugbank.ca/drugs/DB00852
https://www.ncbi.nlm.nih.gov/pubmed/7056280
http://www.jaci-inpractice.org/article/S2213-2198(15)00252-4/fulltext
https://www.chpa.org/SalesVolume.aspx
http://www.phillymag.com/sponsor-content/otc-medications-allergy-symptoms/
