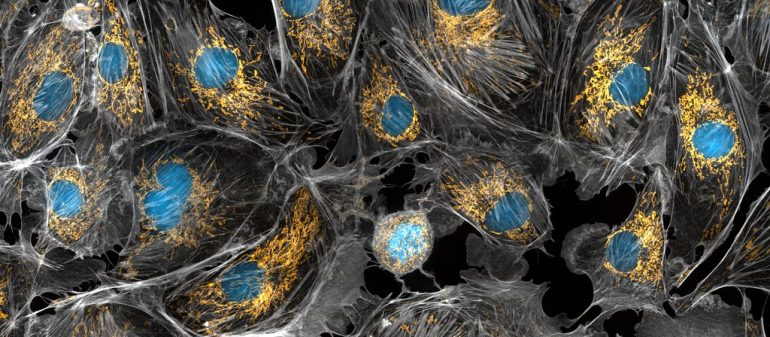
In every elementary and middle school science class, students are taught that mitochondria are the powerhouses of the cell. Textbooks often portray these organelles as brightly colored structures with a myriad of layers and filaments. However, while mitochondria may be important for providing energy for cells, they are also vastly entangled in a wide variety of other functions and may even be critical to disease progression.
Neurodegenerative disorders are some of the most prevalent and fatal diseases in the United States. Neurodegenerative disorders are diseases in which cells of the central nervous system stop functioning properly or die, causing issues in communication between brain cells. This increased miscommunication between cells may subsequently result in drastic changes within an individual, including altered speech, movement, and memory functions. These changes are characteristic of common neurodegenerative diseases, including disorders such as Parkinson’s and Alzheimer’s.
But how could such small organelles like mitochondria be accused of causing neurodegenerative disease? As surprising as it sounds, mitochondria actually play large roles in influencing the trajectory of disease progression across various neurodegenerative disorders. Neurons consume over a quarter of the glucose produced by the body and require a large amount of energy to function. They depend on mitochondria to provide this energy.
In addition to fueling neurons, mitochondria also play critical roles in functions specific to preventing the onset of neurodegenerative disease. For example, mitochondria are also implicated in cell metabolism. The ATP produced by mitochondria is used to maintain ion gradients and homeostasis in our cells.
Ok, so mitochondria are clearly important to neurological function, but what happens when they stop functioning properly? In order to investigate the answer to this question, several studies have examined mitochondrial dysfunction and found that it is closely correlated to neurodegeneration.
When mitochondria are damaged or do not function properly, they may increase oxidative stress within a cell. Oxidative stress refers to an unbalanced amount of free radicals, or molecules that have unpaired electrons. Free radicals are harmful because they are highly reactive and may harm various parts of the cell by removing electrons from cell structures. In fact, free radicals have been found to inflict damage to proteins, DNA, and cell membranes by this mechanism. Thus, as mitochondrial damage is closely related to increased oxidative stress, it can also be correlated to an accumulation of damage to the cell. . This increased cell damage may accelerate nerve injury and may then lead to various diseases over time.
Furthermore, mitochondrial dysfunction can result in the release of proteins which may stimulate premature cell death and further disease progression. Mitochondrial dysfunction is similar to an earthquake that shakes and damages the cell. Similar to when an earthquake occurs and leaves damage in its wake, mitochondrial dysfunction sends out a wave of particles and proteins that destabilize the entire cell.
However, just like how cities prepare for earthquakes by implementing various safety protocols and procedures, cells prepare to manage the effects of mitochondrial damage and dysfunction through mitochondrial quality control. Mitochondrial quality control is a mechanism by which damaged and misfolded mitochondria are identified and removed. These mitochondria are identified through various processes specific to each quality control mechanism and removed by proteins such as autophagosomes. Through the removal of these organelles, the harmful effects stimulated by damaged mitochondria are prevented, safeguarding the integrity and health of the cell and promoting neuron survival. When mitochondrial quality control is disrupted in neurons, it may result in altered neuron function and even lead to neurodegeneration. In fact, many neurodegenerative diseases correspond to alterations in mitochondrial quality control mechanisms.
There are many different types of mitochondrial quality control mechanisms in neurons. Mitophagy, or selective mitochondrial degradation, is one of the most prevalent mechanisms for removing damaged or dysfunctional mitochondria. One common mitophagy mechanism is through the Parkin/PINK1 pathway. This pathway is critical to preventing the onset of neurodegenerative diseases such as Parkinson’s disease. In fact, pathogenic pathways in Parkinson’s disease are closely associated with decreased mitochondrial quality control function.
But how does this pathway work? In healthy mitochondria, the PINK1 gene is cleaved. However, in dysfunctional mitochondria, the PINK1 gene is not cleaved and produces a protein that accumulates on damaged mitochondria. This protein functions in a pathway that ultimately leads to the degradation of damaged mitochondria–so let’s dive into the molecular mechanisms underlying this process.
First, the initial accumulation of PINK1 leads to the activation of the ubiquitin and Parkin proteins, which are subsequently recruited to the respective mitochondrial site. The PINK1 protein acts as a messenger that calls for backup to help remove damaged organelles.
Once all the proteins arrive at the site, they work together to deal with the damaged organelle. The Parkin protein binds to the ubiquitin protein, facilitating the development of ubiquitin chains. Ubiquitin is closely involved in the destruction of damaged proteins and organelles. Subsequently, these ubiquitin chains amplify the strength of ubiquitination signals and increase Parkin activity, which in turn increases ubiquitination of certain substrates and amplifies the feedback loop. Accordingly, mitochondria surrounded by ubiquitin chains are tagged for degradation. Similar to using a megaphone to make a voice louder for everyone to hear, these proteins use ubiquitin chains as a megaphone to let the cell know that the mitochondria should be degraded.
Once the cell hears these signals, it will send over the necessary organelles to degrade the mitochondria. In this case, autophagosomes contain the necessary cellular machinery and materials to degrade defective organelles, and will selectively identify ubiquitinated mitochondria. Following initial identification, the autophagosomes will proceed to degrade and remove the dysfunctional mitochondria.
Although the PINK1/Parkin pathway appears to be an effective mitochondrial quality control mechanism, there exist many other types of mitochondrial quality control processes. Some of these alternate mechanisms include the formation of mitochondrial vesicles. When mitochondria are damaged, they may release their damaged components through extracellular vesicles, otherwise known as mitochondrial-derived vesicles (MDVs). But why would the cell use this mechanism instead of the PINK1/parkin pathway? After all, the PINK1/parkin pathway is a reliable mechanism to remove damaged mitochondria, so there should be no need to spend cellular resources on another mechanism.
The uniqueness of this particular mechanism lies in the fact that it allows for the mitochondria to remain functional by only selectively degrading certain parts of the organelle instead of degrading the entire mitochondria. Another benefit to this mechanism is that once MDVs are released, they are often removed by a lysosome as opposed to an autophagosome. Lysosomes simply break up the harmful components in the MDV, allowing the cell to potentially reuse them in other processes, whereas autophagosomes fully degrade and remove mitochondria.
Therefore, it is clear that mitochondrial quality control mechanisms are of vital importance to preventing mitochondrial and cellular dysfunction in neurons and, in turn, preventing the onset of several neurodegenerative diseases. However, what happens when mitochondrial quality control stops functioning properly? As you might have guessed, the answer involves the improper functioning of neurons and implications in neurodegenerative diseases. Studies have found that in Alzheimer’s disease, mitochondria are often characterized by various mitochondrial DNA mutations, abnormal gene expression, and an increase in amyloid β peptides. These peptides can cause mitochondrial damage and hinder mitochondrial function. An accumulation of these particular peptides is also common in Alzheimer’s disease and can significantly alter mitochondrial dynamics.
Mitochondrial quality control mechanisms are imperative to preventing the onset of neurodegenerative diseases and unintended cell death. Therefore, these mechanisms present tremendous potential in the development of new treatments or prevention methods for progressive neurodegenerative diseases. While many people reduce the role of mitochondria to simply being the “powerhouse of the cell,” they are really so much more! These purple, layered organelles might be imperative to preserving neurons and thus contributing to the ability to function in day-to-day activities.
References:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3056539/
- https://kids.frontiersin.org/articles/10.3389/frym.2018.00070
- https://www.frontiersin.org/articles/10.3389/fnins.2018.00342/full
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3056539/
- https://journals.physiology.org/doi/full/10.1152/ajpcell.00222.2006#:~:text=mitochondria%20are%20unique%20organelles%20providing,with%20ATP%20by%20oxidative%20phosphorylation.&text=This%20immense%20metabolic%20demand%20is,cell%20membranes%20and%20for%20neurotransmission.
- https://www.sciencedirect.com/science/article/pii/S0005272810005797
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2234350/
- https://www.metabolismjournal.com/article/S0026-0495(00)80077-3/pdf
- https://hopes.stanford.edu/about-free-radical-damage/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2234350/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2234350/
- https://www.frontiersin.org/articles/10.3389/fnins.2018.00342/full
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5302033/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4441056/
- https://www.cell.com/molecular-cell/comments/S1097-2765(15)00662-0
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5446078/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7290979/
- https://www.sciencedirect.com/science/article/pii/S2213231714001189
- https://www.nature.com/scitable/topicpage/the-discovery-of-lysosomes-and-autophagy-14199828/#:~:text=Farquhar%20observed%20these%20closed%20vesicles,autophagy%22%20(Figure%201)
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3321185/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4746252/
- https://pubmed.ncbi.nlm.nih.gov/26589414/