By Joyce Sunday | SQ Features Writer | SQ Online (2015-16)
Five years ago, she was diagnosed with stage two HIV infection and placed on antiretroviral drugs. After failing to keep up with her initial medication schedule, she was given another set of medications. Her new antiretroviral drugs were meant to be taken every day at specific times, but she found it difficult to maintain this complicated schedule. In addition to struggling with the scheduling of her medications, she had trouble performing certain tasks that involved critical thinking and comprehension. Finally, she visited the doctor, who informed her that unfortunately, she was having serious neurological side effects from the HIV medication. Despite great advances in the HIV field, neurological disorders associated with HIV infection and antiretroviral drugs have not been adequately addressed.
HIV is contracted through the exchange of bodily fluids, like milk, blood, or semen, during activities such as breastfeeding, sexual intercourse, and sharing infected needles. This virus affects helper T cells, which defend the body against pathogens such as bacteria. The virus usually destroys the infected cell them during this replication process. In this stage of HIV infection, a person can experience flu-like symptoms, like fever, dry cough, and fatigue. Once the helper T cell count drops significantly, patients become susceptible to minor infections that a healthy immune system could normally handle. This stage of HIV is known as acquired immune deficiency syndrome (AIDS).
While there are antiretroviral drugs that help HIV patients live normal lives, there are many downsides to living with the virus, including neurological problems associated with both the infection and its medications. Recently, more scientists have begun to concentrate on understanding the neurological issues of HIV patients. One of the major players in the field of HIV neurology is Dr. Ronald Ellis, a professor of neuroscience at UC San Diego and the co-director of the HIV Neurobehavioral Research Programs (HNRP). During his interview with the chair of neurosciences, Dr. William Mobley, Dr. Ellis stated that, despite the utilization of antiretroviral medication to treat HIV infection, neurologic diseases associated with the disease have not been addressed. Although some HIV patients have a suppressed viral load due to their medication, they are still prone to have neurological disorders. When HIV enters the body and travels through the blood brain barrier to the central nervous system, it causes an inflammation which damages the spinal cord, brain and hinders neurons from properly functioning. Some antiretroviral drugs which result in neurological complications are significantly influenced by genetics.
HIV neurological diseases may not necessitate hospitalization, but they can significantly decrease the quality of life of HIV patients.According to Dr. Ellis, a person who suffers chronic effects of HIV infection can have “two most common life-changing conditions, which are mild cognitive impairment and neuropathy” because of the damages done to the peripheral nerves. Neuropathy can affect knowledge, creativity, cognition, critical reasoning, vigor, energy, and mental conditioning. These neurological conditions can also affect patients’ abilities to take their medications as these drugs require intricate schedules. If an HIV patient does not strictly adhere to their medication schedule because of psychological issues, they may require new medicine that can prevent their virus from developing resistance to their old medication.
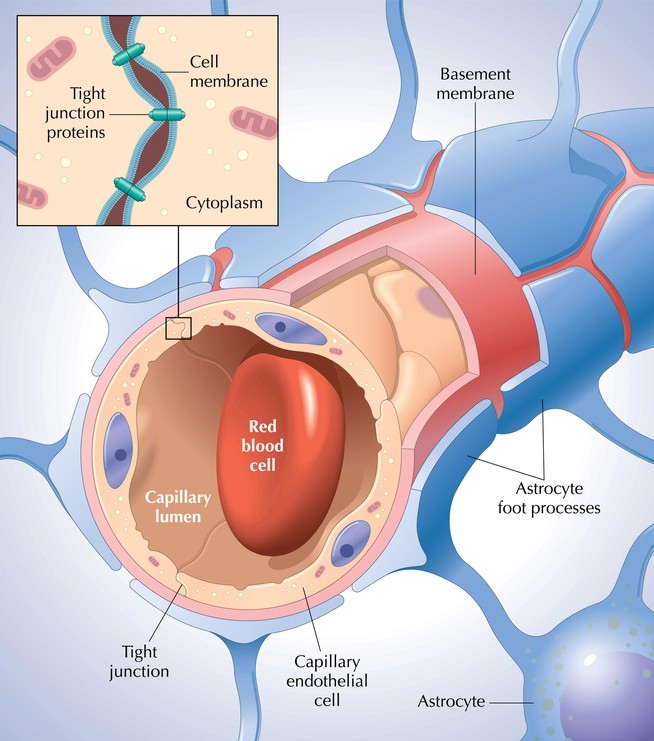
Dr. Ellis has several solutions to make these cognitive problems less severe. One is treating the nervous system directly. One obstacle to this is the central nervous system’s blood—brain barrier (BBB), which defends the brain by preventing substances from flowing to the brain from the blood. Certain types of treatments and medications, like chemotherapy and antiretroviral drugs, cannot penetrate into the brain because the cells that make up the capillary walls of the BBB are firmly and securely closed. The medications that can cross the BBB would be able to reach target tissues in the brain and help with treating cognitive and neurological disorders.
[hr gap=”0″]
SOURCES:
- https://www.aids.gov/hiv-aids-basics/hiv-aids-101/how-you-get-hiv-aids/
- http://www.biology.arizona.edu/immunology/tutorials/aids/hivimmune.html
- http://emedicine.medscape.com/article/1167008-overview
- http://www.southernresearch.org/life-sciences/infectious-diseases/virology/retroviruses-hivsiv
- http://neurosciences.ucsd.edu/centers/hiv/Pages/about.aspx
- https://cias.rit.edu/faculty-staff/101/faculty/340
- http://neurosciences.ucsd.edu/faculty/Pages/ronald-ellis.aspx
- http://www.avert.org/hiv-and-aids-treatment-care.htm
- http://www.merckmanuals.com/home/brain-spinal-cord-and-nerve-disorders/biology-of-the-nervous-system/brain
- http://www.aidsmap.com/Why-taking-your-HIV-treatment-properly-is-so-important/page/1327020/
- http://www.avert.org/stages-hiv-infection.htm
- http://www.hopkinsmedicine.org/healthlibrary/conditions/nervous_system_disorders/neurological_complications_of_hiv_134,46/