Let’s talk about poop. Every day, we ingest food. Whether it’s from your favorite taco truck or your own kitchen, we need to eat to survive. So, how does this meal transform into energy?
The enzymes of the gastrointestinal tract (GIT) act as biological catalysts to aid in the breakdown of food until they are small enough to travel through the bloodstream and be transported across the cell membrane. What if we zoom in? Amid all of the acid, cells, and enzymes, there are hundreds of bacteria species harbored within our GIT, forming what is known as the gut microbiome. The gut microbiome is instrumental in digestion as it aids in the breakdown of sugar polymers, proteins, and some fats into more manageable sizes for enzymes. Providing non-nutrient essential factors and occupying a pivotal ecological niche that is responsible for immunosurveillance of harmful pathogens, the gut microbiome not only aids the GIT but is also responsible for the development of our immune system! When we excrete waste, a lot of gut microbes are present in our poop.
However, the bacterial diversity in our poop today is astoundingly low compared to that of our ancestors. Per a study published in Nature magazine, researchers analyzed the DNA of 8 excavated ancient coprolites (fossilized feces) of animals that lived many years ago. They are considered “trace feces,” which means that they aren’t the remains of an animal’s body itself, but rather something that came from an animal. Coprolites can be useful in identifying species that existed during a particular time period and can give clues about an animal’s diet, habitat, and the ecological system it inhabited.
These particular coprolites were excavated from rock shelters in Northern Mexico and Southwestern America a few years ago, having been preserved in a moisture-free, stable-temperature environment. A research team led by Aleksandar Kostic, an assistant professor of microbiology at Harvard Medical School, radiocarbon dated these samples to somewhere between 0 C.E and 1000 C.E. Radiocarbon dating is a method that provides an age estimate to carbon-based materials that originated from living things. This technique uses the radioactive isotope of carbon (carbon-14), a species of the chemical element carbon with an unstable nucleus that emits radiation. A sample’s age can be estimated by measuring the amount of carbon-14 present in it. Given the age estimate of these coprolites, the researchers speculated that the feces were the excrement of the indigineous people who lived in Northern Mexico and Southwestern America at the time.

After deducing the age of the desiccated feces, the researchers sought to analyze the contents of the coprolites. Specifically, they were curious about which species of bacteria and microorganisms were present in this ancient excrement. The researchers rehydrated small bits of the feces to soften the cell membranes of the bacteria so they could extract and recover long strands of DNA.
The differences found in the microbial populations of paleofeces (a.k.a. the coprolites) and the average poop of today’s humans were astounding. Many unfamiliar, novel bacterial species were discovered in the coprolite samples that simply do not exist in today’s gut. Interestingly, 40% of the microbiome were new bacterial species. This led the researchers to conclude that the human gut has experienced a mass extinction event over the past millennia, meaning we have lost nearly half of the diversity in our gut over the generations. But how has this extinction affected us? Is it negligible because microorganisms are so small, or is it significant because they play a large role in our survival?
The dissimilarities in microbial diversity between ancient and present-day poop can be tied to many factors; one such factor is our diet. In ancient cultures, nutrition was primarily derived from farming, hunting, and gathering, which promoted the growth of a wide range of microbial species in the human gut. The types of microbes found indicated that the ancient diet consisted of high-fiber foods such as maize and beans.
In contrast, humans in the industrialized world consume the “grocery store diet” that consists of processed foods, low nutrition, and unvarying food habits. Although we consume a variety of dishes, lasagna isn’t very different from a burger because they both predominantly contain wheat. Kostic reasons that we have lost a large portion of our microbial population because our gut environment is too constant in contrast to that of our ancestors who had a dynamic gut environment due to their frequent change in habitat and variety of foods.
In an environment marked by change, microorganisms have the space to mutate and adapt to new environments through the use of transposases. Transposases are enzymes that catalyze the movement of DNA to another part of the genome. They encourage the formation of new variants that perform different functions and contribute to a diverse ecosystem. However, humans today do not have pressure to evolve because we have manipulated the natural environment to our comfort; we control the food supply of our ecosystem and have molded it to fit our sedentary lifestyle, leaving no space for the adaptation or improvement of the gut microbiome: a choice that is leading us to deteriorating health and increased disease susceptibility. However, other disparities in microbiome diversity cannot be attributed solely to our diet – so what other factors affect our microbial population?
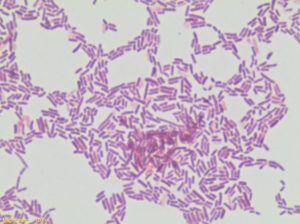
An example of a bacterium found in the coprolite samples is Treponema succinifaciens. This bacterium has been found in the gut of many traditional and rural populations, but is entirely absent in any urban and Western populations likely due to an increase in antibiotic use. Imagine that you punch a wall very forcefully. The most likely outcome is that you will break your fingers the first time. But if you keep punching a wall every day, eventually you will build up enough strength to be able to punch a wall and not break your fingers. Antibiotic resistance works very similarly. Developed during the industrial revolution, medicines called antibiotics were manufactured to kill bacteria. Unfortunately for humans, bacteria mutated and developed resistance to antibiotics. The organisms that adapted to tolerate the effects of the antibiotics were “naturally selected” and produced offspring. These “stronger” species became more prevalent and others lacking this resistance became obsolete, thus wiping out many species of bacteria over time and drastically changing the microbiome composition in our gut.
Industrialization also engendered the concepts of sanitation and food processing. The rise in harsh chemical compounds destroyed kingdoms of bacterial species. Processing food with innumerous preservatives became profitable for sellers and convenient for buyers. But at what cost did we gain cleanliness and convenience? Increasing the shelf life of food in the manner that is done today kills all chances for microbial growth. Without bacteria, digestion is arduous, disease is impending, and our immune system lacks necessary support. How do we expect to gain diversity through food if the food we eat doesn’t contain any bacteria at all? The “grocery store diet” is one of the main causes for the drastic drop in diversity, and the less diversity we have, the less adversity we can battle. So, what are the “good germs” we need to have in order to fight off the “bad germs”? For example, the bacteria S. thermophilus produces large quantities of the enzyme lactase, making it effective in the prevention of lactose intolerance. Many strains of the species Bifidobacterium and Lactobacillus act as probiotics and shield us against harmful infections and conditions such as diarrhea and colon inflammation caused by “bad germs” such as Clostridium difficile and Helicobacter pylori. Hence, to cater our diet in promoting a diverse gut microbial community of “good germs,” we need to incorporate foods that have a high fiber content and that do not indefinitely sit on shelves.
The researchers also found a connection between the gut microbiome and immunity using the coprolite samples. The DNA from the coprolite samples had a lower number of genes that produce proteins specialized in degenerating the protective mucus layer of the small intestine. Mucus is our primary line of defense against pathogens: it traps, disables, and lyses germs that attempt to enter our body. Without it, we would be susceptible to a much larger spectrum of bacterial and viral diseases. Also, certain microbes present in the industrialized gut hinders the development of a strong immune system and leads to a higher incidence of chronic diseases such as type 1 diabetes, autoimmune diseases, and allergies.
The gut microbiota that colonizes the GIT showcases coevolution, which is the influence of closely associated species on each other’s evolution in a symbiotic environment benefiting both parties. But what would happen if this system is not balanced? Known as dysbiosis, disequilibria between the host and intestinal microbiome leads to hazardous inflammatory health conditions, such as Crohn’s and IBS, and can promote carcinogenic (cancer-causing) activity leading to oncogenesis (development of tumors).
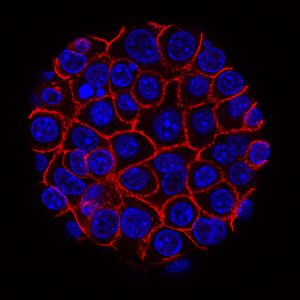
A recent study published in Science Translational Medicine discusses the role gut microbiota plays in curing cancer. Specifically, the gut microbiome population can be manipulated and used therapeutically to reduce the incidence of certain tumors, improve the effectiveness of anti-cancer agents, and optimize the effects of chemotherapy. Ongoing studies have also found correlations between the composition of the gut microbiome and diabetes (type 1 and type 2), further emphasizing that research into the human gut microbial populations can be transformational in the medical field.
Given the vast applications of understanding the gut microbiome, it is important that we delve deeper into understanding how different bacterial species affect the functions in our body. If we can cultivate these species in the lab, we can understand their physiology in more depth. This would give us the tools needed to engineer and manipulate our existing gut microbiota to cure chronic illnesses, cancer, and other calamitous diseases.
References:
- https://hms.harvard.edu/news/guts-our-ancestors
- https://www.science.org/doi/10.1126/science.372.6543.671
- https://www.nature.com/articles/s41586-021-03532-0
- https://www.nature.com/articles/s41586-018-0620-2
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4566439/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4878258/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4690201/
- https://www.science.org/doi/10.1126/scitranslmed.3010473?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed
- https://www.healthline.com/nutrition/gut-microbiome-and-health#TOC_TITLE_HDR_5
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7415231/
- https://www.britannica.com/science/radioactive-isotope
- https://www.sciencedirect.com/science/article/pii/S2052297518301008
- https://en.wikipedia.org/wiki/Antimicrobial_resistance#Natural_occurrence