BY ANJALI IYANGAR | SQ ONLINE REPORTER | SQ 2019-2020
Over the course of the last few months, discussion about the COVID-19 pandemic has been one of the things at the forefront of the public sphere, whether it be conversations at the dinner table about exponential growth of cases, news channels continuously airing coronavirus stories, or friends reminding you of CDC guidelines to prevent the spread of the SARS-CoV-2 virus. Amidst all the panic and grim news surrounding the coronavirus pandemic, one hopeful news story about a different virus has been overshadowed. This is the story of the second ever human immunodeficiency virus (HIV) patient that has been cured.
In early March 2020, it was announced that Adam Castillejo, a man from London, was the second person ever to be cured of HIV. Just as the first patient (Timothy Ray Brown, or the “Berlin patient”) was cured, Castillejo was given a stem cell transplant leading to the mitigation of HIV in his body. This amazing news comes nine years after the cure of Mr. Brown. In the history of the disease, why have there only been two people ever cured? In order to understand this question, we must consider some background information about HIV.
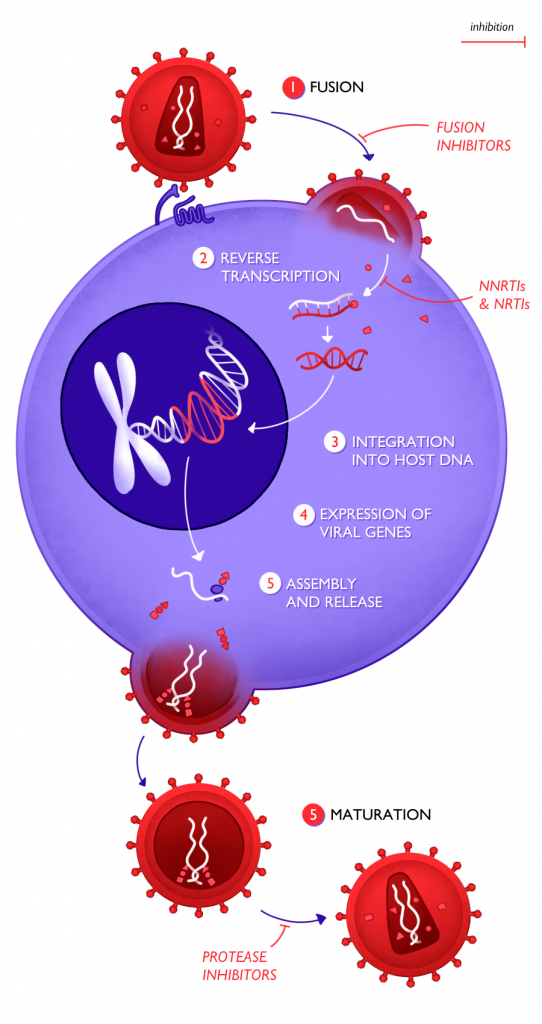
HIV spreads via bodily fluids and infects its host’s immune system. In a healthy immune system, immune cells called CD4 cells, or helper T cells, help mediate the body’s immune response. HIV targets and enters these CD4 cells, using their machinery in order to replicate itself. HIV is an RNA retrovirus, meaning that the genetic material of the virus is stored in single-stranded RNA. Upon entering CD4 cells, an enzyme called reverse transcriptase reverse transcribes the viral RNA into double-stranded DNA. Essentially, this enzyme reverses the process of transcription in which DNA is copied into RNA. By copying viral RNA into DNA, reverse transcriptase provides a mechanism by which viral genes can be integrated into the host CD4 cell’s genome. After the viral DNA of HIV has integrated into the DNA of the CD4 cells, more copies of the virus are created by the host cell itself. The newly created viruses can then leave the host CD4 cell to infect other CD4 cells and continue this process.
What makes HIV such a complex virus is the insidious cycle that it initiates. HIV affects the immune system by using cells of the immune system as hosts to grow and replicate in. However, in order to fight the virus, the body naturally increases its immune response by creating more CD4 cells. Essentially, the virus exploits this process by using the cells of the immune system as a means to proliferate. Consequently, completely eliminating the virus becomes very difficult.
While a cure which completely eliminates the virus (the cause of the disease) does not currently exist, treatments can mitigate symptoms of the disease by preventing the virus from replicating. The current treatment for HIV, antiretroviral therapy (ART), is a concoction of drugs that prevents HIV from replicating in host CD4 cells. Two classes of drugs that are part of ART are nucleoside reverse transcriptase inhibitors (NRTIs) and non-nucleoside reverse transcriptase inhibitors (NNRTIs). As the names suggest, both NRTIs and NNRTIs work by inactivating the reverse transcriptase enzyme of HIV that converts viral RNA into DNA. If this process of converting viral RNA into DNA is stopped, viral DNA is unable to integrate into host DNA and therefore halts the production of more copies of the virus. Yet another class of drugs in ART is protease inhibitors, which prevent the maturation of newly released HIV. Fusion inhibitors are an additional class of drugs in ART that prevent HIV from entering CD4 cells. As their name suggests, fusion inhibitors bind to a protein on the viral membrane’s surface in order to prevent fusion between the CD4 cell membrane and the viral membrane. The last class of drugs that are used in the treatment of HIV are CCR5 antagonists, which bind to CCR5 receptors on CD4 cells. HIV uses CCR5 receptors as a key to get inside CD4 cells; however, if CCR5 receptors are blocked, HIV will be unable to bind to and enter CD4 cells. All the aforementioned drugs decrease the viral load of HIV and are effective as treatment if taken regularly. However, no known drugs can permanently cure the disease, as the viral load will increase again once ART is stopped.
The two men that have been cured of HIV up to this date were both given stem cell transplants to treat their cancers. Castillejo, the most recently cured patient, was suffering from lymphoma, which prompted a bone marrow transplant. Through this transplant, Castillejo’s immune cells (which included HIV-infected CD4 cells) were replaced with donor cells. The structure of the donor’s CD4 cells enabled this transplant to cure Castillejo’s HIV. In the transplanted donor cells, the specific gene that encoded for the CCR5 protein on the surface of CD4 cells was mutated. As this is the protein primarily used as a receptor for HIV to enter CD4 cells, replacing the patient’s cells with the donor’s cells prevented the virus from entering Castillejo’s cells, thus curing him. Not only did the transplant remove most infected cells, but it also replaced them with ones that structurally could not be entered and hijacked by HIV. After this transplant, however, Castillejo was not immediately considered to be cured. It was not until Castillejo had stopped taking ART for seventeen consecutive months following the transplant (without detectable levels of viral load resurfacing) that he was declared cured.
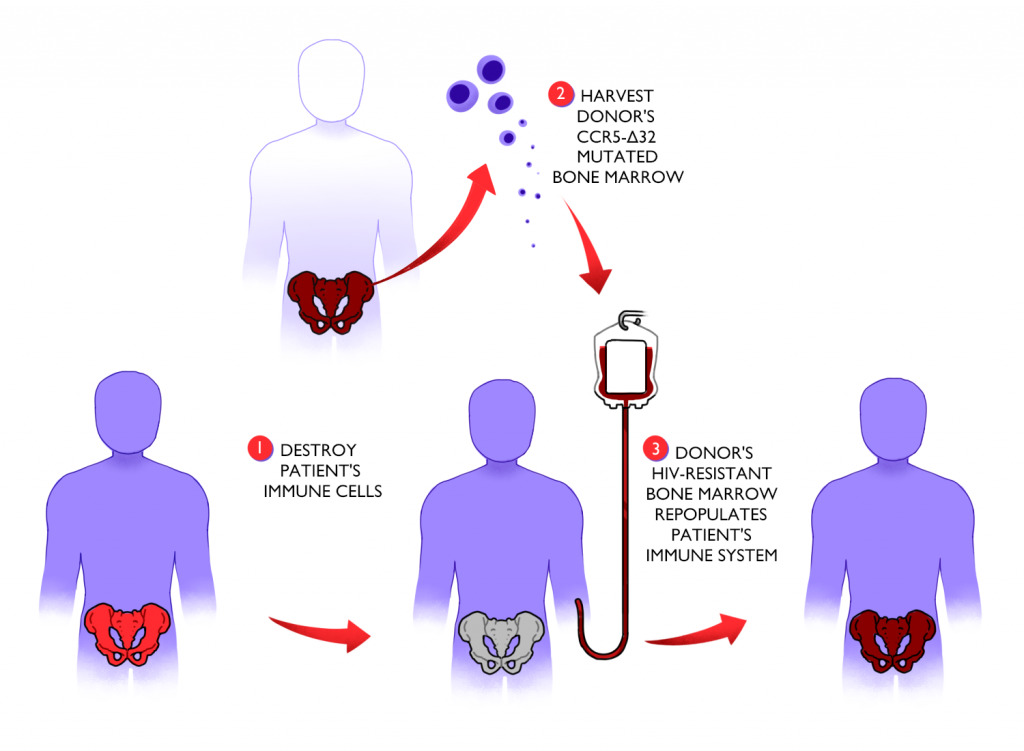
In spite of these two patients’ success stories, the extreme complications associated with stem cell transplants makes them infeasible as a large-scale solution for HIV patients. Both patients cured of HIV thus far received this treatment not for their HIV but as a form of therapy for their cancers. Nevertheless, abundant research is being done regarding other avenues for a possible HIV cure, such as gene therapy targeting CCR5 receptor genes. Regardless of the limited applicability of stem cell transplants as a standard cure for HIV patients, the story of Mr. Castillejo serves as a hopeful reminder of the possibility of scientific progress in the treatment of epidemics.
Sources:
- http://i-base.info/guides/art-in-pictures/the-hiv-lifecycle-in-detail
- https://www.medicalnewstoday.com/articles/2nd-person-cured-of-hiv-thanks-to-stem-cell-transplant
- https://www.livescience.com/second-person-cured-hiv-adam-castillejo.html
- https://www.nytimes.com/2020/03/09/health/hiv-aids-london-patient-castillejo.html
- https://www.thelancet.com/journals/lanhiv/article/PIIS2352-3018(20)30069-2/fulltext#back-bib4
- https://www.bbc.com/news/health-51804454
- https://www.nytimes.com/2019/03/04/health/aids-cure-london-patient.html?action=click&module=RelatedLinks&pgtype=Article
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4143801/
- https://aidsinfo.nih.gov/understanding-hiv-aids/glossary/1650/viral-suppression
Illustrations by Ellis Zhang.