Ancient Greece was one of the first places where the spread and control of diseases—otherwise known as epidemiology—were studied. Greek physician Hippocrates was named the Father of Medicine for his work toward understanding the logic behind sickness. He believed illness was caused by an imbalance in the body’s four humors: blood, phlegm, yellow bile, and black bile, and that in order to cure someone, a certain humor needed to be added or removed to rebalance the body. Hippocrates was also the first person to explore and analyze the relationship between environmental influences and the distribution of diseases. Through this exploration, Hippocrates coined the terms endemic—a disease that is regularly present within a particular community—and epidemic—a disease that is suddenly widespread in a community.
Additionally, Hippocrates supported a theory of disease known as the miasma theory. This theory claimed that diseases, like the Black Death, were caused and spread by miasma, or polluted vapors rising from sewers and swamps. This theory was widely accepted in places like Europe and China and defined the understanding of disease until the mid-nineteenth century. However, an English physician named John Snow was always a bit skeptical of the theory.
When Snow was just an apprentice, a cholera—an illness defined by symptoms of vomiting and diarrhea—epidemic hit London, England. Snow helped to treat the patients, who were mostly coal miners. When the epidemic ended, the physicians concluded that it was caused by miasmas. Snow, on the other hand, was unconvinced. It did not make sense to him that the majority of cholera victims were coal miners, and yet, there were no sewers or swamps underground in the mines. About sixteen years later, after Snow had become a physician himself, there was another outbreak of cholera in London. Still doubting the miasma theory, Snow began to track the spread of the disease himself. He discovered that the first contractor of cholera was a seaman who quickly died in a room he rented in London. Snow also uncovered that a different man who rented the same room also contracted cholera and died by interviewing his doctor. To Snow, this was evidence that some kind of contagion or germ—a microscopic organism previously theorized to spread disease—was the cause. As he continued examining cholera patients, he noticed that all their symptoms consisted of digestive discomfort. This further disproved the miasma theory in Snow’s mind because if the disease was spread through polluted air, then symptoms should appear in patients’ airways, not their digestive systems. As a result, he began to theorize that cholera must be being spread by polluted water or food, and the disease contagion may be present in the discharge of the patients, like vomit or diarrhea. Snow worked to track the disease around London, mapping down the water facilities near high cholera mortality rates. Eventually, Snow wrote and published a pamphlet named On the Mode of Communication of Cholera detailing all his evidence that cholera is a germ that is spread through contaminated water systems and sewers. Although his theory was largely ignored at the time alongside the other scientists and physicians who proposed similar ideas, it eventually helped to form our current understanding of the spread of disease: the germ theory.
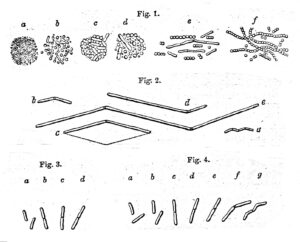
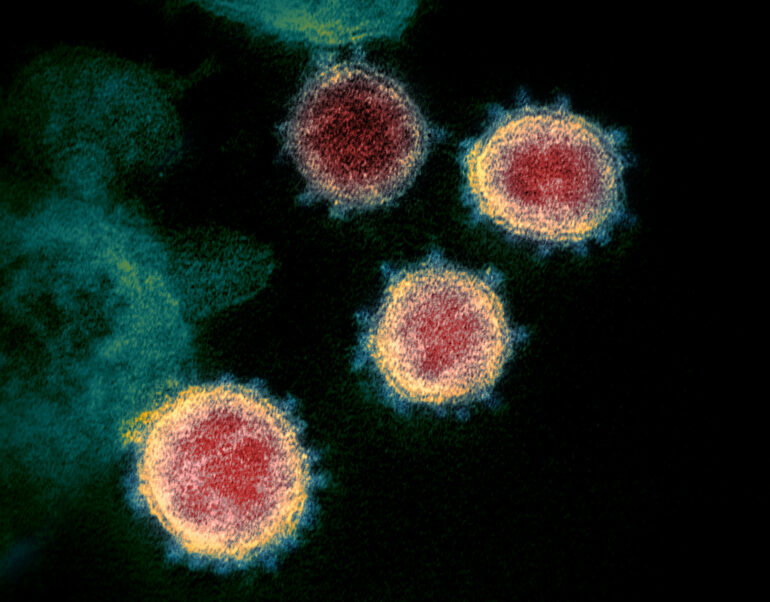
Image: Early illustrations of germs (Source)
Today, it is accepted that microscopic organisms, known as germs, are the cause of the spread of diseases largely because of John Snow’s work on tracking cholera and identifying its cause. Furthermore, he laid the foundation for the field of epidemiology which can be seen in how the Centers for Disease Control and Prevention (CDC) handles disease outbreaks. The most recent example of this is when the CDC investigated the cause and spread of the coronavirus, an epidemic spread around the world, otherwise known as a pandemic. After the initial outbreak of COVID-19, epidemiologists began to work toward identifying its source by surveying the communities in which it was prevalent, similar to Snow. However, unlike Snow, modern-day epidemiologists were able to more efficiently track COVID-19 cases via public health surveillance systems (i.e. symptom reports from state health departments and health care systems), making it much easier for them to not only determine its symptoms like coughing and congestion but also its mode of transmission: airborne virus. Additionally, this data was used by epidemiologists and biostatisticians—statisticians that work with data specific to biological organisms—to predict the spread of the coronavirus via the SIR—susceptible, infectious, removed—epidemiological model. Essentially, this model divides the population into three categories: yet to be infected (susceptible), infected (infectious), and no longer infected (removed). Each category is defined by a set of equations that are used to determine the estimate of people in each category at certain points in time. Epidemiological models were used to determine the effectiveness of non-pharmaceutical prevention methods. For example, epidemiologists used COVID-19 transmission data and statistics from previous endemics to predict that masks and social distancing via lockdowns would help slow down the spread of the airborne disease.
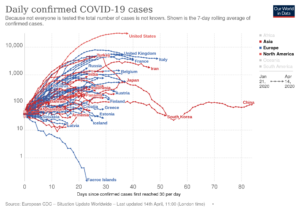
Image: Graph of Daily COVID-19 cases in 2020 (Source)
The field of epidemiology has clearly advanced quite a lot since John Snow’s time. However, the basic principles of his work with cholera are still prevalent in how epidemiological studies are done today. While current epidemiologists have much more advanced methods of data collection and interpretation, they are still tracking disease to its most concentrated locations in order to better understand it, just like Snow did when he tracked the cholera-contaminated water sources. When looking at how much his methods still influence the current study of the spread of disease, it is clear why John Snow was rightfully named the Father of Modern Epidemiology.
Sources:
- https://www.emro.who.int/emhj-volume-23-2017/volume-23-issue-12/the-forgotten-history-of-pre-modern-epidemiology-contribution-of-ibn-an-nafis-in-the-islamic-golden-era.html
- https://bio.libretexts.org/Bookshelves/Microbiology/Microbiology_(Boundless)/10%3A_Epidemiology/10.01%3A_Principles_of_Epidemiology/10.1A%3A_History_of_Epidemiology
- https://www.ph.ucla.edu/epi/snow/choleratheories.html
- https://www.ph.ucla.edu/epi/snow/fatherofepidemiology.html
- https://www.ph.ucla.edu/epi/snow/mapsbroadstreet.html
- https://curiosity.lib.harvard.edu/contagion/feature/germ-theory
- https://www.mayoclinichealthsystem.org/hometown-health/featured-topic/endemic-epidemic-pandemic
- https://www.cdc.gov/coronavirus/2019-ncov/science/about-epidemiology/index.html
- https://www.cdc.gov/coronavirus/2019-ncov/covid-data/faq-surveillance.html
- https://www.maa.org/press/periodicals/loci/joma/the-sir-model-for-spread-of-disease-the-differential-equation-model
- https://www.nature.com/articles/d41586-021-00183-z