Introduction
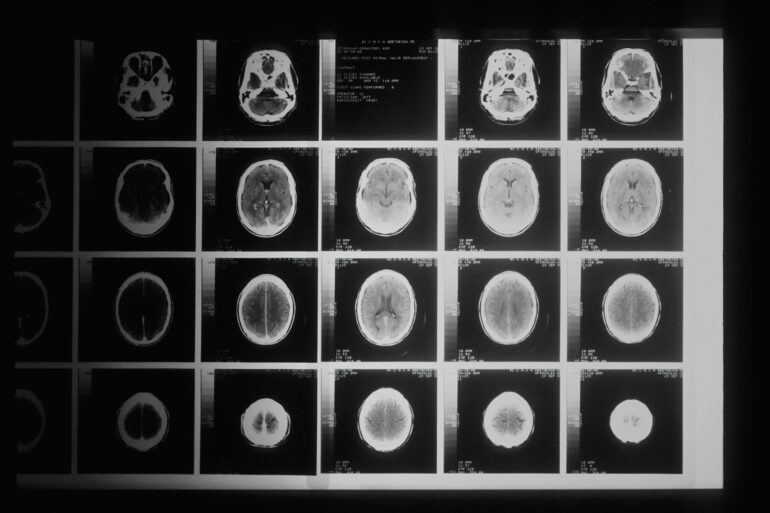
Sometimes, when people say the problem is in your head, it can be literal. Maybe the problem is your head: more specifically, your brain. Treating conditions in the brain is difficult— chemical and surgical approaches pose potential complications to this sensitive location. When it comes to treating brain cancer, the situation gets no easier.
Brain cancer poses many complications for creating treatment plans. Glioblastoma, the most common form of brain cancer in adults, is a non-metastatic tumor that forms in soft tissues of the brain, meaning that the tumor stays localized in the brain and does not spread throughout the body. Due to the delicate nature of the tumor’s location (i.e the high risk of neurological damage), treatment plans often fall short of complete remission and carry notable side effects and risks. However, new research from the University of Connecticut proposes a novel solution that not only makes treatment less invasive and more effective, but has the potential to redefine how we create new treatments for conditions like brain cancer.
Problems with the Solutions: Current Drawbacks in the Standard of Care
For treatment of glioblastomas, surgical resection and chemotherapy are often used in tandem to reduce tumor size. Surgical resection involves removing a tumor entirely or removing as much cancerous tissue as possible. However, surgery is challenging for glioblastomas, due to both location (the brain) and the high amount of vascularization that characterizes this type of tumor. Vascularization refers to the network of blood vessels and capillaries that connect to a tumor, providing oxygen-rich blood. These vessels creates a complex surgical field in an already delicate location. Additionally, any damage to healthy, non-cancerous brain tissue may risk neurological impairment.
Chemotherapy is another common approach to reduce tumor size. Chemotherapy refers to combinations of anticancer drugs that kill cancerous cells. While chemotherapy effectively reduces tumors, it has its drawbacks. While killing cancerous cells, chemotherapy also kills healthy, non-malignant cells, resulting in side effects such as fatigue and nausea. Chemotherapy may also impact immune function, as it can damage bone marrow, leading to a decrease in white blood cell count. For glioblastomas, chemotherapy is less effective, as the anticancer drugs have difficulty surpassing the blood brain barrier. The blood brain barrier is a network of blood vessels surrounding the brain that regulates the passage of large or polar molecules into the brain. While the blood-brain barrier protects the brain from toxins and viruses, it also means that large molecules in chemotherapies cannot completely penetrate the brain to reduce tumors effectively.
While surgery and chemotherapy can shrink tumors, they do not always result in complete removal of the tumor, and challenges unique to glioblastomas make these approaches less effective. With existing efforts to make more effective surgical practices and drugs present, some seek a different approach: making the body more effective at fighting cancer.
Breaking Down Barriers: High Intensity Ultrasound and the Blood Brain Barrier
To address the drawbacks with current treatment methods, researchers turn to a new way of improving drug efficacy: increasing the permeability of the blood-brain barrier by exposing the brain to high-intensity focused ultrasound (HIFU).
HIFU is defined as targeted, high-frequency sound waves that have therapeutic effects in soft-tissue tumors like those found in breast and prostate cancers. The heat from the sound wave kills cancer cells and their vascular systems, and exposure to ultrasound frequencies can make cell membranes more permeable, increasing the efficacy of drug uptake. However, HIFU cannot pass through air or solid bone, which could seemingly bar its use for the treatment of brain cancer. However, Dr. Thanh Nguyen from the University of Connecticut has proposed a solution. Instead of working through the skull, get the ultrasound to work inside of it.
Implanted Innovation: Therapeutic Frequencies
Getting ultrasound waves into the human brain is a daunting and invasive task. Implanted ceramic ultrasounds have been utilized before to make chemotherapy more effective, however, these devices require two invasive surgeries (one for implantation, and one for removal). The Nguyen lab works to address this problem, creating an implanted ultrasound that is biodegradable.
In order to find a material that can emit an ultrasound frequency and harmlessly dissolve within the brain, the Nguyen lab turned to a property known as piezoelectricity. Piezoelectricity is the ability of a material to emit a frequency after being stimulated with an electric current. One material with this property is glycine, a common amino acid that is biodegradable. However, engineering with glycine can be difficult; it is a brittle material that shatters easily. To overcome this, Nguyen and his team decided to embrace glycine’s temperamental nature, and intentionally grew and shattered glycine, creating microscopic crystals. They then processed the crystals with a biodegradable polymer known as polycaprolactone to create a biodegradable and piezoelectric film, generating ultrasound waves with the same intensity as a traditional ceramic implant.
When tested in mice, the use of this ultrasound drastically increased the efficacy of paclitaxel (PTX), a therapeutic agent for brain cancer that has difficulty surpassing the blood-brain barrier in an entire dose. When PTX was used in tandem with the ultrasound, it was significantly more effective, with mice showing marked tumor reduction and increased life expectancy. Additionally, no adverse effects of the device were found 6 months after initial implantation. The implanted ultrasound has now moved into safety and efficacy testing in large mammals. These results not only suggest promise for future use of this ultrasound against glioblastomas, but also open the door for similar ultrasound-based technologies for neural conditions beyond cancer.
Increasing the Frequency: New Waves in Cancer Treatment
The success of this device creates questions about the future of cancer treatment. It is unknown whether patients will embrace surgery for implantation when known surgeries for resections exist. Additionally, the potential accessibility of this device or how it would affect existing chemotherapy regimens is unknown. While there are questions regarding the dissemination of this technology and its public reception, it is certain that the approach behind the implant has the potential revolutionize treatment development for diseases like cancer. Rather than searching for newer, more effective drugs, making the body more efficient and surpassing elements like that of the blood-brain barrier through interdisciplinary approaches may be the key to therapeutic advancements. By working to tackle the source of an issue through therapeutics, engineering has the potential to idealize medical research. As Dr. Nguyen’s work demonstrates, the solution can be bioengineered, and may even end up being all in your head.
Sources:
- https://www.ncbi.nlm.nih.gov/books/NBK469987/
- https://unsplash.com/photos/a-black-and-white-photo-of-various-mri-images-BDKid0yJcAk