When you hear the word “parasite,” what comes to your mind? With all the buzz around the recently revived “Alien” franchise, it’s easy to envision dangerous, otherworldly creatures like facehuggers, chestbursters, and more. Sensational as these creatures might seem, parasites themselves aren’t that far removed from our reality. According to the National Institute of Health, humans are infected with nearly 300 species of parasitic worms and over 70 species of protozoa, or unicellular organisms. While a small, infamous fraction impacts human health through devastating disease, others can give us unexpected health and societal benefits. For example, in a study done in 2007, multiple sclerosis patients experienced a significantly lower number of relapses after they were infected with intestinal parasites. Farmers also use parasitoids to exterminate pests that would otherwise destroy millions of pounds’ worth of crops every year. Already, we have discovered purposes for parasites in our bodies and food, but what about in our medicine?
One of the most prolific parasites present in humans is Toxoplasma gondii, a single-celled intestinal parasite infamous for its ability to infect most warm-blooded animals. While cats are their definitive hosts, T.gondii is estimated to infect around a third of the global human population. Thankfully, most infections caused by T.gondii, known as toxoplasmosis, are asymptomatic given a healthy immune system. However, severe infection can manifest as life-threatening brain inflammation or eye infection. Much of the research on T.gondii has focused on merely uncovering its methods of invasion and survival, but some researchers saw beyond the biology and dared to dream. After over a decade of work, researchers Shahar Bracha at Tel Aviv University and Lilach Sheiner at the University of Glasgow have successfully engineered T.gondii to deliver therapeutic proteins directly to the brain.
The Challenge of Protein Therapeutics
To understand how innovative their accomplishments are, one must know the context of protein therapeutics. The overall goal is to replace or supplement the proteins that become abnormal or deficient due to disease. For example, a biosimilar protein is manufactured to mimic the functions of naturally-found proteins involved in the immune response. However, its utilization becomes difficult, as a protein’s journey to a target cell or location is fraught with many potential roadblocks. Exposure to protein-degrading enzymes, low pH, and the instability of its subunits all increase the possibility of denaturation, or irreversible unfolding. A major sector of protein and antibody therapeutics research aims at treating the wide spectrum of brain disease, from neurodegeneration to cancer. In the case of protein delivery to the brain, the ultimate challenge lies in passing the highly selective blood-brain barrier (BBB). The tightly packed endothelial cells of the BBB serve to prevent larger, potentially dangerous substances from entering blood vessels. Unfortunately, this may also impede the passage of potentially helpful proteins and peptides.
How T.gondii Delivers Proteins
What is remarkable about T.gondii is that it has “co-evolved” with its hosts to be able to bypass the BBB and infiltrate the brain. The exact and entire method utilized by T.gondii to infect the central nervous system remains unclear; however, one strongly proposed mechanism involves hijacking immune cells that cross the BBB, allowing for rare, but sufficient, instances of T.gondii entry. Once inside a host cell, T.gondii secretes a variety of effector proteins that facilitate its survival and growth through altering host cell functions or attacking host cell defenses. Fascinated by this parasite’s abilities, microbiology researchers Bracha and Sheiner began to explore possible methods for manipulating T.gondii to deliver proteins of their choosing. They directed their attention to T.gondii’s two primary modes of protein secretion: the rhoptry system and the dense granule system. Composed of a bulb and sac, the rhoptry organelle discharges proteins into the host cell’s cytosol, or intracellular fluid, through transient openings in the cell’s plasma membrane. With this method, there is no need for a full-on cell invasion, and each parasitic unit can inject multiple cells. Conversely, the dense granule system uses the host cell’s plasma membrane to form a bubble-like sac called a parasitophorous vacuole within the host cell. The original T.gondii cell will reside in this vacuole and carry out long-term protein secretion until it can replicate to infect other host cells. With this knowledge, the researchers selected one effector protein from each secretion system to use as a carrier for their target therapeutic proteins, almost like a parasite’s parasite! By utilizing T.gondii’s versatile secretion systems, the researchers achieved successful protein delivery into a variety of media such as human neurons and human brain organoids, as well as in vivo in mice. They even engineered certain T.gondii strains to deliver two different targets using both rhoptry and dense granule systems simultaneously.
Successful Protein Delivery with T.gondii
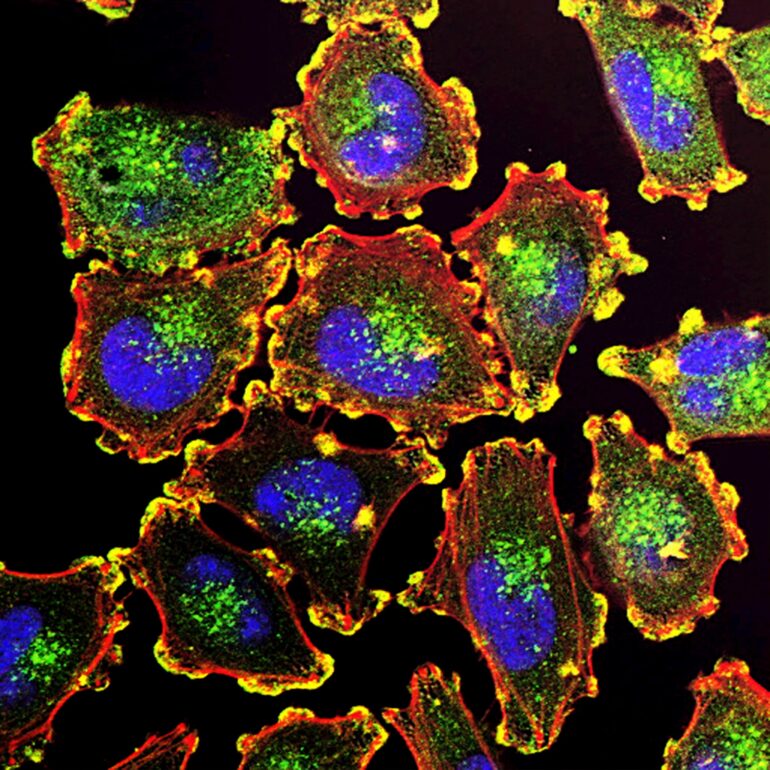
In their paper, Bracha and Sheiner demonstrated successful in vitro delivery of crucial therapeutic targets for diseases like spinal muscular atrophy, Rett syndrome, and lysosomal storage disease–all via T.gondii-based vectors. The researchers further investigated the delivery and functionality of MeCP2, the Rett syndrome target protein, in neuronal cell cultures and brain organoids. MeCP2 expression plays a key role in neuronal differentiation and cell-to-cell communication, and mutations of the MeCP2 gene are strongly associated with many neurodevelopmental disorders like Rett syndrome or autism. To quantify the delivery levels of MeCP2, they used T.gondii to infect mature human neurons without the gene needed to produce the MeCP2 protein, meaning that they don’t naturally contain MeCP2. Then, they stained and compared the infected neurons to neurons with natural levels of MeCP2, or MeCP2-positive neurons. Just 24 hours after infection, protein levels in the MeCP2-infected neurons already reached 58% of protein levels in the MeCP2-positive neurons. These results are incredibly promising and similar to those from previous studies utilizing viral gene therapy to combat Rett syndrome.
Future Implications of Parasite-Based Protein Therapeutics
Innovative studies like this lay the groundwork for more generalized and robust methods of protein delivery, which are highly relevant for both research and medicine. In the future, executing an efficient delivery of protein targets in vivo would enhance researchers’ ability to manipulate biological processes and observe the effects in a natural context. Bracha and Sheiner’s work provides a preliminary proof-of-concept for the use of T.gondii as a “versatile protein vector” for therapeutic targets at large, and in the brain no less! The focus of future development of their method should be on mitigating the safety risks of potential parasitic infections if this method is implemented in vivo. Although they engineered their T.gondii strains to produce an asymptomatic infection in mice, achieving control mechanisms similar to those used in viral therapies will be pivotal for future medicinal applications. Humans have always had this ingenuity that allows us to integrate the natural world into different facets of our society. We are always forming meanings and discovering new perspectives on what’s around us. Take the meaning of a parasite, which can range from an unearthly organism to a deep-rooted insult for a person. It is possible that in the future, the connotation of “parasite” will shift positively with the widespread use of parasite therapeutics.
Citations:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC126866/
- https://www.nhm.ac.uk/discover/positive-parasites.html#:~:text=When%20tapeworms%20and%20roundworms%20set,t%20get%20out%20of%20hand.
- https://www.sciencedirect.com/science/article/abs/pii/S0165572811000051#:~:text=Farez%2C%202007
- https://pubmed.ncbi.nlm.nih.gov/19433092/
- https://www.ncbi.nlm.nih.gov/books/NBK7752/
- https://www.ema.europa.eu/en/human-regulatory-overview/biosimilar-medicines-overview#:~:text=in%20the%20EU-,A%20biosimilar%20is%20a%20biological%20medicine%20highly%20similar%20to%20another,medicines%20to%20cause%20an%20immune
- https://www.sciencedirect.com/science/article/abs/pii/S1740674909000043?via=ihub
- https://www.cell.com/trends/parasitology/fulltext/S1471-4922(22)00033-2#:~:text=Mechanisms%20proposed%20for%20T.,parasitized%20leukocytes%20(Trojan%20horse)
- https://www.sciencedirect.com/science/article/pii/S0944501319304719
- https://www.nature.com/articles/s41564-024-01750-6
- https://journals.plos.org/plospathogens/article/figures?id=10.1371/journal.ppat.1006351
- https://www.news-medical.net/news/20190620/Dangerous-brain-parasite-invades-host-cell-maintains-steady-nutrient-supply.aspx
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5798978/
- https://www.nature.com/articles/s41564-024-01772-0/figures/1