Introduction
When one is sick, the comforting mentality tends to be: “When I get better…” The focus shifts to improvement—the cough will abate, the fever will break, and eventually, the illness will become a thing of the past. But what if there was no hope of this relief? For those with conditions like Alzheimer’s disease, or AD, there isn’t. AD is a neurodegenerative disease that leads to loss of cognitive function, including loss of memory and reasoning, behavioral changes, and eventually, loss of brain volume. AD affects more than 6 million individuals in the United States and is the leading cause of dementia. For those with AD, current treatments cannot offer hope of improvement—any cognition lost will remain lost.[1] The best a patient or their family can hope for is a slower rate of cognitive decline: abilities will remain slightly longer and their loved one will lose cognition at a slower rate. But what about AD makes it so difficult to restore cognition?
AD is characterized by an accumulation of beta-amyloid protein plaques and neurofibrillary tau tangles in the brain.[2] Beta-amyloid plaques and tau tangles are dense aggregates of malformed proteins. The build-up of these insoluble protein aggregates has devastating effects on neurons. Neurons are the cells in the brain responsible for sending electrical and chemical signals that carry information that is essential for cognitive processes like memory. In addition to forming these insoluble plaques, beta-amyloid proteins also take a soluble form in the brain. These soluble proteins become toxic when they aggregate in excess, as in AD brains. Beta-amyloid protein aggregation occurs at synapses, or the gaps between neurons where inter-neuron signaling takes place. This aggregation then disrupts neuron signaling. The combination of neuron death and synaptic damage leads to the loss of cognitive function, eventual loss of brain volume, and death, characteristic of AD. However, it is worth noting that not all instances of beta-amyloid presence are known to cause Alzheimer’s, and that beta-amyloid accumulation has been found in brains that did not demonstrate a cognitive deficit.[3]
A Promising Start: The Dore Lab and PSD-95
Rather than focusing on beta-amyloid plaques, Dr. Kim Dore and her lab focus on the synapse. More specifically, the proteins around the synapse, like scaffolding proteins (proteins responsible for maintaining molecular spatial arrangements). The Dore Lab specifically investigates a scaffolding protein known as postsynaptic density protein 95 (PSD-95), which is a key element responsible for synaptic transmission. By altering PSD-95 expression in AD model mice, the Dore Lab demonstrated that levels of PSD-95 are directly correlated with synapse health and cognitive ability and even have the potential to undo the damage caused by AD: a previously unattainable feat. Levels of PSD-95 were measured through cognitive tests in mice and through post-mortem electrophysiological imaging of brain tissue samples. These results suggest that increasing levels of PSD-95 may provide a novel path towards increased cognition in patients.
Scaffolding Proteins and PSD-95
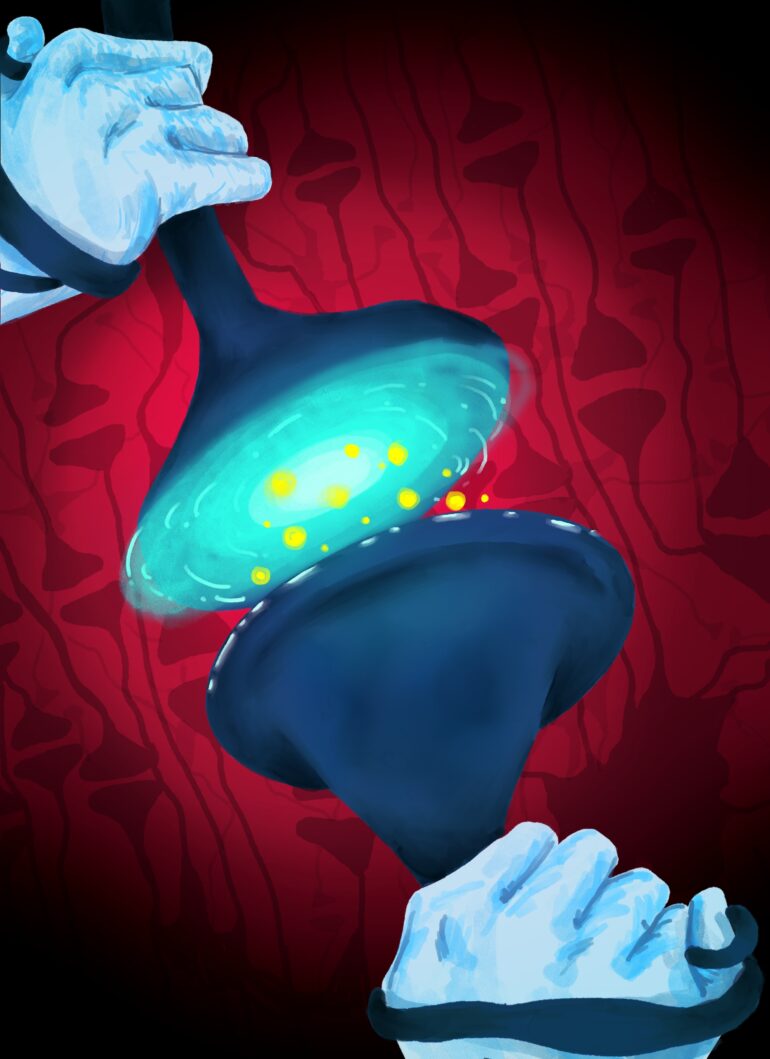
Scaffolding proteins like PSD-95 are a family of proteins responsible for coordinating the activity of signaling molecules. These proteins bind to these molecules and associate them with their intended receptor, enabling the specificity of a signaling pathway.[4] PSD-95 is a scaffolding protein that acts at the N-methyl D-aspartate (NMDA) receptor. NMDA is a key receptor that helps mitigate the impact of beta-amyloid on the synapse by blocking the impact of beta-amyloid on the spatial arrangement of the NMDA receptor. It is the conformational change induced by beta-amyloid on NMDA that correlates with loss of synapse function.[5] The essential neurotransmitter glutamate acts at the NMDA receptor, and exposes the neuron to calcium in the process.[6] In brains affected by AD, excess glutamate exposes the brain to damagingly-high levels of calcium, causing cognitive decline.
Maintaining Receptor and Synaptic Health
Maintaining receptor and synaptic health for as long as possible can slow decline. However, the presence of PSD-95 alone is not sufficient to maintain synaptic health: only palmitoylated PSD-95 remains at synapses. Palmitoylation is the process of adding fatty acids, like palmitic acid, to proteins. Not all forms of PSD-95 interact with the NMDA receptor in a way that promotes synaptic health, so it is essential to evaluate levels of expressed PSD-95 as well as levels of palmitoylation.
PSD-95 and the AD Brain
To evaluate the effect of PSD-95 on AD brains, the Dore Lab induced the expression of PSD-95 in advanced AD-model mice, which are animals that have developed AD over a period of months and exhibit a marked decrease in cognitive function. To monitor and compare changes in cognitive function, baseline cognitive ability was established through performance in a memory test. Mice with increased PSD-95 levels expressed a greater ability to remember and successfully locate the platform compared to control mice.[7] In human patients, cognition is tested via multi-part recall tests and task assessments, such as a patient’s ability to draw a clock.[8]
These cognitive tests are not the only way to evaluate the impact of PSD-95 on an AD brain. Post-mortem imaging of brain tissue samples from PSD-95-increased mice showed increased dendritic spine health compared to control mice.[7] Dendritic spines are extensions of neurons that act as markers for synaptic health: increased amounts of spines correlate to more functional synapses.[9] The larger presence of dendritic spines in mice with increased PSD-95 indicate its restorative effect on the AD phenotype, and validate the improved cognitive ability of PSD-95 treated mice.
Factors Affecting PSD-95 Activity
Several factors beyond expression impact PSD-95 activity at the synapse. For example, the upregulation of protein kinase C alpha (PKCα) reduces the functionality of PSD-95.[10] While the exact mechanism behind this interaction is not fully understood, the overall result is an increase in synaptic depression (lowered levels of neurotransmitter release) and more cognitive decline.[11] However, there are mutations known to lead to PKCα upregulation, but they are not therapeutically viable targets because genetic editing is not currently a clinically viable solution. The Dore Lab has found an approach that is accessible today: addressing the process of palmitoylation, or protecting levels of functional PSD-95.
Moving Forwards: Thinking Clinically
As the relationship between PSD-95 and cognition becomes increasingly clear, the focus now turns to maximizing its application. This research not only provides a path to create potential therapeutics for patients suffering from AD, but may also provide insight into the biological mechanisms behind the range of impacts AD has on different patients. Dr. Dore and her team discovered that only female mice were impacted by increased levels of PSD-95. The reason for this difference remains unexplained; however, this discrepancy aligns with another observed disparity AD. Women are more likely to get Alzheimer’s disease than men, making PSD-95 an incredibly effective treatment for a more at-risk population.[12] Reasons behind this disparity are currently being explored.
Final Takeaways
For too long, AD treatment and research approaches have focused only on slowing disease progression with little consideration of restoring ability. The work of the Dore Lab with PSD-95 provides an approach that restored cognitive function to AD-model mice within five days. This novel approach of addressing the mechanism behind the most devastating symptom of Alzheimer’s (cognitive decline), rather than its fundamental cause (plaques), may be the answer to improve quality of life in those living with this devastating disease. While genetic editing to alter human PSD-95 levels is not currently feasible, depalmitoylation enzymes might be a clinically viable target. For patients who have never before had the comfort of recovery, the work done by the Dore Lab provides hope that those suffering from Alzheimer’s can indeed bounce back.