BY AISHWARYA VUPPALA | UTS WRITER | SQ 2017-2018
[hr gap=”null”]
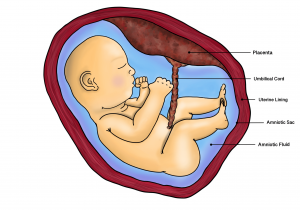
“Push, push … it’s almost out!” Most pregnant women hear this phrase when giving birth to their child, but they actually hear it for a second time before pushing their placenta out. Unbeknownst to many, the placenta serves as the connection between the mother and the baby; the umbilical cord is attached to the baby’s side of the placental disc and the maternal side of the disc is attached to the uterine lining1. It has been established that placentas are crucial to the baby’s growth in the womb, but they can also cause preeclampsia in the mother during and after pregnancy. The placenta is a membrane through which substances, including nutrients and oxygen, can be transported from the mother to the baby2. Therefore, its level of functioning also affects placental development, the baby’s growth, the mother’s blood flow, and other important processes. Keeping this statement in mind, placental pathology indicates that a particular feature of preeclampsia is a lack of proper blood transportation between the mother and the baby due to the functional failure of the maternal arteries in the placenta4. Researchers and medical specialists have been able to identify a few biological causes which can lead to inadequate development of blood vessels.
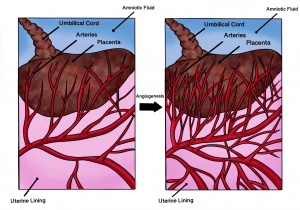
Angiogenesis is the development of new blood vessels, which is especially crucial to the placenta. As mentioned before, when this process is disturbed, it can potentially lead to preeclampsia. Abnormalities of angiogenic factors have been witnessed to contribute to preeclampsia. One example is the increased production of the antiangiogenic protein sFlt1, which inhibits vascular endothelial growth factor and placental growth factor signaling. When uninhibited, proper endothelial development includes the growth of a layer of cells on the placenta as well as the growth of several blood vessels throughout the organ. Essentially, this deficiency in endothelial growth disrupts the development of the blood vessels; therefore, this antiangiogenic protein is indirectly responsible for obstructing the transportation of materials across the placenta6. Although certain factors like sFIt1 have been discovered to lead to the development of preeclampsia, there are several similar contributing factors that exist, some of which are unknown. This makes preeclampsia difficult to treat, as the cause of the condition cannot be easily identified.
As of now, there no medications that directly treat preeclampsia, and pretty much the only treatment is to deliver the baby if the symptoms become severe7. Some of these symptoms include high blood pressure, headaches, changes in vision, seizures, swelling, and the presence of protein in the urine3. Sometimes antihypertensive medications may be administered to lower blood pressure, and medications like magnesium sulfate are given to women experiencing seizures7. These symptoms can often lead to illness and even death for the mother and unborn baby, which is why most hospitals make sure to monitor the mother’s symptoms during the pregnancy. In fact, maternal death rates are higher among women with early onset (12.2 per 100 deliveries) and late onset preeclampsia (5.5 per 100 deliveries) than among women without preeclampsia (3 per 100 deliveries)5. Understanding the placenta is key to comprehending preeclampsia, and that is what researchers are aiming to do in order to prevent potentially fatal consequences. Despite these observations, there are still other aspects of preeclampsia that need to be understood in order to predict and prevent the disease earlier in pregnancy.
Clinical criteria, such as high blood pressure and headaches, aren’t enough to diagnose the disease because sometimes women are misdiagnosed, as they could have these symptoms due to other health conditions6. Although monitoring symptoms can help diagnose preeclampsia, pathologists also have been gathering and analyzing placental samples to isolate any morphological differences between normal and preeclamptic placentas. These samples are used to also validate diagnoses of preeclampsia made based on symptoms during the pregnancy. Essentially, disruptions in placental development are what lead to preeclampsia, but preeclampsia can have several causes related to many unknown and known cellular and mechanistic disruptions. Although the placenta plays a big role in reproduction and preeclampsia, the inner workings of this organ are still very much unknown; however, there is a lot of research regarding the placenta and preeclampsia currently taking place around the world including at UC San Diego in the Parast Lab8. Finally, to all the pregnant women out there and those who anticipate pregnancy in their future: take the time to learn more about preeclampsia while also being observant of symptoms during pregnancy in order to get proper medical attention.
Sources:
- http://www.med.umich.edu/lrc/coursepages/m1/embryology/embryo/06placenta.htm
- http://www.biologydiscussion.com/human-development/placenta-structure-and-functions-explained-with-diagram/5163
- https://www.preeclampsia.org/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3381433/
- http://journals.lww.com/greenjournal/Abstract/2014/10000/Maternal_Morbidity_Associated_With_Early_Onset_and.18.aspx
- http://hyper.ahajournals.org/content/63/2/198.full
- https://www.nichd.nih.gov/health/topics/preeclampsia/conditioninfo/Pages/treatments.aspx
- https://parastlab.wordpress.com/publications/
- https://outsideitselectric.wordpress.com/2015/03/07/placenta-tree-of-life-prints/
Illustrations by Sara Kian