By Julia Brown | UTS Staff Writer | SQ Online (2014-15)
For cancer patients and their families, it often seems as though living well and comfortably is a cry into the void. In the United States, in particular, the feat is virtually impossible. Many people, public and professional alike, attribute rising healthcare costs to factors such as malpractice, the obesity problem, a larger number of people going to see their doctors, the cost to educate doctors, the idea that the U.S. is simply a wealthier nation and should pay more because of that.5 Some, as in one study by the McKinsey Institute, point out that one of the more major reasons, it seems, is that with the exception of programs such as Medicare, price negotiations for medical care are not well-regulated by the government.2 Providers essentially have the ability to charge prices as high or low as they desire, resulting in a market which does not often consider the impact on the patient.6
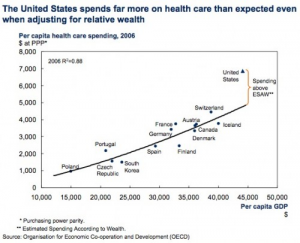
However, according to Boston University health economist Austin Frakt, the complexity of the issue is in that each one of these factors plays a role, and each one does not solely account for the enormous cost disparity, shown in Figure 1 to the left, between the United States and similar countries.5 This makes it incredibly difficult to pass legislation on, and even more difficult for those affected by the increasing costs, so as a result, many families have to pay a lot of money for medications and services that might not even help very much.The question of the healthcare crisis then shifts from “Can we solve it?” to “While the inefficiencies of the system exist, is there a way to help patients and their families choose their medications more wisely so they can minimize their financial burden?”
A recent study at the UC San Diego School of Medicine seems to have answered this question to some extent, at least for patients and families of patients dealing with cases of the most prolific and aggressive form of brain cancer in humans, glioblastoma. Glioblastoma patients commonly undergo a method of chemotherapy using pills of a chemical known as temozolomide. For each recurrence of the tumors, the medication can cost tens of thousands of dollars.4 However, the medication only produces long-term effects in about 10—15 percent of patients to whom it is administered.1 As treatment options continue to advance and become more numerous, especially with these low improvement statistics, it becomes more important for patients and their families to choose their treatments wisely so as to not waste time and money on options that are less likely to be effective.
Prior to the study, the presence of the enzyme MGMT was linked with a lower efficiency of temozolomide.3 This meant that if the researchers could determine the concentration of MGMT in and around a tumor, they could ascertain the effectiveness of temozolomide therapy for a given patient.

The researchers performed a screen of the entire human genome to examine the effects of certain microRNA molecules, which can act like on and off switches for genes. The researchers were able to identify the specific molecules that regulate MGMT in glioblastoma cells. As shown by Figure 2 to the right, one particular type, microRNA-603, was shown to suppress MGMT by a large margin. This allowed the medication to dramatically decrease the amount of cancer cells.2 In other words, if a patient has a lot of this type of microRNA, temozolomide therapy has a good chance of working. This means that assessing the types and amounts of microRNA molecules present in a patient can help the patient and their family determine whether the predicted effectiveness is worth the cost or they should consider a different form of treatment.
Indeed, as this is one of the first studies to have conducted a genome-wide screen for MGMT regulators,2 it may be a while before this practice of using microRNA molecules to predict temozolomide efficiency is readily available in hospitals. When it is, however, it will be a significant step toward helping glioblastoma patients fight for their health without breaking the bank.
As for rising healthcare costs in the U.S. as a whole, there is not any one simple answer.5 There are innumerable factors, including malpractice, education of doctors, and lack of price regulation, that contribute to the problem in big ways and in small, and there exists a lot of disagreement as to which factors are more important than others. With virtually no end in sight to the high costs of healthcare in the United States, studies like this give patients a chance to make their financial burdens a bit more worth enduring.
[hr gap=”0″]
References
- “Biomarker Predicts Effectiveness of Brain Cancer Treatment.” UC San Diego Health System. University of California, San Diego, 01 July 2014. Web. 09 July 2014.
- Farrell, Diana, Eric Jensen, Bob Kocher, Nick Lovegrove, Fareed Melhem, Lenny Mendonca and Beth Parish. “Accounting for the cost of US health care: A new look at why Americans spend more.” McKinsey Global Institute. McKinsey & Company, December 2008. p.66. Web. 08 August 2014.
- Kushwaha, Deepa, Valya Ramakrishnan, Kimberly Ng, Tyler Steed, Thien Nguyen, Diahnn Futalan, Johnny C. Akers, Jann Sarkaria, Tao Jiang, Dipanjan Chowdhury, Bob S. Carter, & Clark C. Chen. “A genome-wide miRNA screen revealed miR-603 as a MGMT-regulating miRNA in glioblastomas.”Oncotarget [Online], 5.12 (2014): 4026-4039. Web. 21 Jul. 2014
- Wasserfallen, Jean-Blaise, Sandrine Ostermann, Serge Leyvraz and Roger Stupp. “Cost of temozolomide therapy and global care for recurrent malignant gliomas followed until death.” Neuro-Oncology [Online], 8.16 (2014): 1523-5866. Web. 21 July 2014.
- Frakt, Austin. “What Makes the US Health Care System so Expensive.” The Incidental Economist RSS. N.p., 2 Oct. 2010. Web. 25 Oct. 2014.
- Rosenthal, Elisabeth. “The $2.7 Trillion Medical Bill.” The New York Times. The New York Times, 01 June 2013. Web. 25 Oct. 2014.